Updates from two IAHPC Board Members – India
Palliative Care for Children in a Resource Poor Setting, an Indian initiative
by Dr. Gayatri Palat*

Today, a child diagnosed with cancer in a developed country has an 80% chance of being cured. Unfortunately, this is not true in India where 75,000 children with recorded cancers each year have a survival rate of less than 20%. Furthermore, of the estimated 2.5 million people in India living with HIV/AIDS, 70,000 are children under the age of 15. Less than 0.4% of needy children have access to palliative care programs designed to address their needs.
Palliative Care for Children in the Mehdi Nawaj Jung (MNJ) Institute of Oncology (MNJIO), Hyderabad
The MNJ Institute of Oncology is a 300 bed tertiary care hospital in the state of Andhra Pradesh, India (population of 65 million). Every year the hospital sees around 1,000 children with cancer.
Most of the children require long, intensive curative treatment. Enormous suffering results from painful procedures, undesirable symptoms and the emotional trauma of facing potentially life threatening illnesses. Many children develop severe anxiety, depression and become withdrawn and non-communicative. Families often travel long distances and stay in the hospital for weeks and when the need for community and family support is greatest, they are totally deprived of it. Very early in our endeavor to cure these children, we realized the dire need for an effective palliative care program for both the children and their families as they confront cancer with all of its physical, psychosocial and spiritual effects.
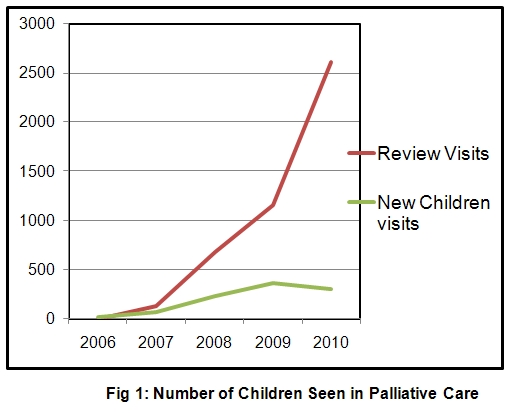
MNJIO Pain Relief and Palliative Care Program, a collaboration of the International Network for Cancer Treatment and Research (INCTR) and Pallium India added pediatric palliative care to their service in 2007. The primary goal of the program is zero-tolerance of pain beginning at diagnosis. Since the pediatric program was established, there has been a rapid increase in the number of children treated beginning with 69 patient visits in 2006 and 2,922 in 2010 ( Fig 1). 70% of children suffered from leukemia and pain was the most common symptom at referral. Other common symptoms included mouth ulcers, constipation, vomiting and tiredness. The total opioid consumption for the year 2010 was 150gms. Every child undergoing interventions such as intrathecal or bone marrow injections received EMLA cream application +/- oral midazolam before the procedure. Other activities included regular weekly support groups, recreational and educational activities, home based care and regular and emergency telephonic consults.
A few successful outcomes of the program have been:
- almost all children receiving cancer treatment and their families are also receiving adequate symptom control and psychosocial support during curative treatment along with a smooth transition to end of life care if required,
- there has been a significant reduction in the dropout rate during treatment, and
- there is good implementation of procedure-related pain relief protocols.
Scope of the program
The pediatric pain and palliative care program is the first of its kind for the entire state of Andhra Pradesh. While the program is currently designed to cater only to the needs of children with cancer, we plan to expand it to include all children living with HIV and AIDS and other life threatening illnesses. A fellowship course in pediatric palliative care will start soon to train specialists in the field.
*Dr. Gayatri Palat is the Program Director for PAX India of the International Network for Cancer Treatment and Research (INCTR). She is currently Associate Professor of the Department of Pain and Palliative Medicine in the MNJ Institute of Oncology in Hyderabad. Dr. Palat is also an IAHPC board member and her biography may be seen at http://www.hospicecare.com/Bio/palat.htm
Medical Council of India (MCI) announces post-graduate course in Palliative Medicine
by M.R.Rajagopal MD

A giant step forward: The Medical Council of India, the statutory body that controls medical education in the country, has approved palliative medicine as a medical specialty and initiated steps to start postgraduate courses about the subject. The entry criterion is a MBBS (the basic medical degree). The three year course will be called "MD in Palliative Medicine". Pallium India submitted a draft curriculum to the Medical Council in 2009; we now expect general discussions to be followed by the emergence of a detailed curriculum. The president of Indian Association of Palliative Care (IAPC), Dr Nagesh Simha, has announced the appointment of an IAPC task force to prepare a draft curriculum to be submitted to MCI.
For a long time, palliative care workers in India have been hoping for approval of Palliative Medicine as a specialty. Doctors working in the field so far have had no academic recognition and could not occupy teaching posts in medical colleges. We believe this positive step will result in a new generation of medical professionals and hopefully an improvement in the quality of palliative medicine practice in the country.
We look forward to a positive development, but we cannot afford to be complacent. So far, palliative care doctors have come into the field largely because they believe in it and are committed to it. Will the MCI's action lead to a new generation of doctors who practice palliative care just as another job? Will there be a fall in the quality of services? This concern is real, and hence non-government organizations in the field have an important task to demonstrate excellent quality care delivery so that it will serve as a benchmark for teaching institutions.
M.R.Rajagopal MD
Chairman, Pallium India
Director, Trivandrum Institute of Palliative Sciences
S.U.T Hospital, Pattom, Trivandrum 695004
Kerala, India
email: [email protected] (Office)
Dr. Rajagopal is also an IAHPC board member and his bio may been read at
http://www.hospicecare.com/Bio/mr_rajagopal.htm
Email this page to a friend!
Top of Page |

